Sepsis, a life-threatening condition resulting from a dysregulated host response to infection, is known to cause widespread endothelial injury and capillary leak. Historically, the treatment approach for sepsis has involved large volume fluid resuscitation to restore intravascular volume and maintain organ perfusion. However, there is growing recognition that excessive fluid administration may lead to fluid overload and related complications. This prompts us to explore the association between positive fluid balance or fluid overload and outcomes in critically ill adults with sepsis, as well as the impact of interventions aimed at reducing fluid balance on patient outcomes.
Numerous studies have investigated the relationship between fluid balance and outcomes in septic patients. These investigations have consistently demonstrated that positive fluid balance is associated with worse outcomes, including prolonged mechanical ventilation, increased length of stay in the intensive care unit (ICU), and higher mortality rates. The mechanism underlying these adverse effects is multifactorial.
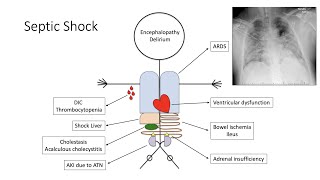
Fluid overload contributes to the development of pulmonary edema, leading to impaired gas exchange and respiratory distress. It also exacerbates organ dysfunction by increasing intra-abdominal pressure and compromising renal perfusion, potentially resulting in acute kidney injury. Furthermore, excessive fluid administration especially with NS can trigger a systemic inflammatory response, worsen tissue edema, and impair microcirculatory flow. These pathophysiological processes collectively contribute to poorer outcomes in septic patients.
In recent years, there has been a shift toward adopting fluid stewardship strategies aimed at optimizing fluid balance and avoiding fluid overload in the ICU. De-resuscitation, which involves a more conservative fluid management approach and goal-directed fluid removal, has emerged as a potential intervention to improve outcomes in septic patients. De-resuscitation involves careful assessment of fluid status, avoidance of unnecessary fluid administration, and early removal of excess fluids through diuretic therapy or renal replacement techniques.
It is important to note that fluid management in sepsis is a complex process that should be individualized based on patients' clinical condition, comorbidities, and response to therapy. The goal is to achieve a euvolemic state, balancing the need for maintaining adequate tissue perfusion while avoiding fluid overload. Regular reassessment of hemodynamic parameters, such as central venous pressure, cardiac output, and urine output, is crucial for guiding fluid management decisions.
In conclusion, accumulating evidence suggests that positive fluid balance and fluid overload are associated with worse outcomes in critically ill adults with sepsis. Interventions aimed at reducing fluid balance, such as de-resuscitation strategies, have shown promise in improving outcomes. However, further research, including large-scale randomized controlled trials, is needed to establish optimal fluid management approaches in septic patients. Clinicians should adopt a judicious and individualized approach to fluid therapy, prioritizing the avoidance of fluid overload while ensuring adequate tissue perfusion in this vulnerable patient population.
#SepsisManagement #FluidResuscitation #FluidBalance #FluidOverload #DeResuscitation #ICUManagement #CriticalCare #EvidenceBasedMedicine #PhysicianPerspective #MedicalResearch #FluidStewardship #SepsisOutcomes #ClinicalInterventions #PatientCare #PhysicianEducation #MedicalEvidence #OptimalFluidManagement #SepsisTreatment #PatientOutcomes









Информация по комментариям в разработке