Dr. Ebraheim’s educational animated video describes the condition of cauda equina syndrome.
Follow me on twitter:
https://twitter.com/#!/DrEbraheim_UTMC
View my profile on Linkedin:
/ nabilebraheim - Everything You Need To Know - Dr. Nabil
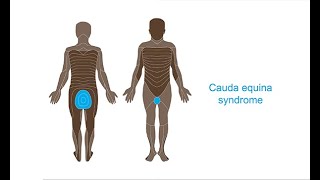
Cauda Equina Syndrome
Cauda Equina Syndrome is a medical emergency, and it must be diagnosed quickly and treated urgently to avoid long term, serious complications. It occurs at the level of the roots causing lower motor neuron injury. The cauda equine is multiple nerve root within the lower end of the spinal canal (beginning at the level of L1). L1-S5 peripheral nerve roots are inside the lumbar canal. Cauda equina syndrome symptoms are usually bilateral and symmetrical. It will be a sudden onset of more back pain than radicular pain, and the sensation over the perianal area is affected. Cauda equina syndrome usually occurs due to a space occupying lesion such as disc herniation, tumor, fracture, epidural hemorrhage or an abscess. Central disc herniation is the most common cause of cauda equina syndrome. Disc herniation can be posterolateral disc herniation, central disc herniation, or foraminal disc herniation. The posterolateral disc herniation is the most common type of disc herniation. With posterolateral disc herniation, there will be a nerve root injury, and there will be changes in the sensory distribution, and there could also be motor and reflex changes. Posterolateral disc herniation usually affects the foot and the ankle. This type of disc herniation is usually treated conservatively initially. Posterolateral disc herniation usually causes unilateral leg pain and weakness with positive straight leg raising test. Central disc herniation will affect the cauda equina. In the cervical spine and in the thoracic spine, compression causes involvement of the spinal cord and an upper motor neuron lesion, but in the lower lumbar spine, compression causes injury to the nerve roots, and it causes a lower motor neuron lesion. In cauda equina syndrome, the patient will have back pain, buttock pain, saddle anesthesia, bilateral leg pain, weakness in the lower extremity, urinary retention followed by urinary incontinence, and bowel dysfunction. Saddle anesthesia occurs from involvement of S2-S5 nerve roots. These nerve roots provide sensory innervation to the anal area, perineum, and inner thigh. Reduced or absent sensation to pin prick in the perianal region from S2-S5 dermatomes. Decreased rectal tone or voluntary contraction. Red flags include lower back pain, sciatica (unilateral or bilateral), sudden sensory disturbances, bladder and bowel dysfunction, and variable lower extremity motor and sensory changes. Early diagnosis is challenging. The initial signal and symptoms usually are subtle. It is important to suspect cauda equina syndrome, and when you do, you should do digital rectal exam and test the perianal sensation. Get an emergency MRI. If you suspect cauda equina syndrome clinically, the MRI should be ordered and read urgently. The patient will probably need to be admitted for completion of the workup. If the patient has a pace maker, then you need to do CT myelogram. If you suspect it, get a study. Identify the source of compression in the lumbar spine. Cauda equina syndrome is a surgical emergency with maximum chance of recovery of the urinary and bowel function with adequate early surgery. The timing of the surgery decides the outcome. The bladder dysfunction symptoms are the least likely to improve, so you want to do the surgery early. You will do early decompression with removal of the disc or bony fragments that is compressing on the nerve roots (very important). The patient should be taken to surgery urgently to provide the best chance of symptoms resolution. Prognosis for cauda equina syndrome, there is improvement in pain and weakness. The result is less predictable for recovery of the urinary bladder and bowel function. If the patient presents more than 48 hours, there will be less than 40% of the patients that have improvement in bladder and bowel function. 60% of the patients will have chronic bowel and bladder dysfunction if surgery was delayed more than 48 hours.








Информация по комментариям в разработке