#ophtalmology #eyes #surgery
#oftalmología #ojos #cirugía
Disease
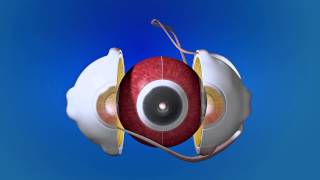
Accumulation of red blood cells within the anterior chamber is referred to as a hyphema. A small amount of blood that is only evident under close microscopic examination is referred to as a microhyphema. A majority of patients present with a history that correlates to the etiology. A history of trauma or recent ocular surgery are the most common risk factors. However, a seemingly spontaneous hyphema can result at times from other causes. Despite the degree or etiology, the management of a hyphema and its associated complications can be challenging for any ophthalmologist.
Etiology
Hyphema can occur after blunt or lacerating trauma, after intraocular surgery, spontaneously (e.g., in conditions such as rubeosis iridis, juvenile xanthogranuloma, iris melanoma, myotonic dystrophy, keratouveitis (e.g., herpes zoster), leukemia, hemophilia, von Willebrand disease, and in association with the use of substances that alter platelet or thrombin function (e.g., ethanol, aspirin, warfarin).[1]
Blunt trauma is the most common cause of a hyphema. Compressive force to the globe can result in injury to the iris, ciliary body, trabecular meshwork, and their associated vasculature. The shearing forces from the injury can tear these vessels and result in the accumulation of red blood cells within the anterior chamber.
Hyphemas can also be iatrogenic in nature. Intraoperative or postoperative hyphema is a well known complication to any ocular surgery. Rarely, the placement of an intraocular lens within the anterior chamber can result in chronic inflammation, secondary iris neovascularization, and recurrent hyphemas, known as uveitis-glaucoma-hyphema (UGH) syndrome.[2] This is a direct result of a malpositioned or rotating anterior chamber intraocular lens. This condition has also been reported in posterior chamber, sulcus, and suture-fixated intraocular lenses.[2][3] Additionally, a hyphema resulting from an ocular laser procedure is a possible adverse event. Postlaser hyphema is not uncommon after the use of the Nd:YAG laser for a peripheral iridotomy. Typically the resulting hyphema is minimal and self-limited.
A spontaneous hyphema, commonly confused with a traumatic hyphema, is likely secondary to neovascularization (eg, diabetes mellitus, ischemia, cicatrix formation), ocular neoplasms (eg, retinoblastoma), uveitis, or vascular anomalies (eg, juvenile xanthogranuloma).[4]
Diagnosis
Diagnosis is made with slit-lamp examination of the anterior chamber. A large hyphema can be noted with pen-light examination alone.
https://eyewiki.aao.org/Hyphema









Информация по комментариям в разработке